The incidence of cutaneous melanoma has increased over the last 25 years but may now be stabilizing. It is estimated that approximately 52,000 new cases will be diagnosed this year in the U.S., resulting in 7,800 deaths attributable to melanoma.
The primary risk factors associated with melanoma are sun, exposure, family history, skin type, pigmentation nevi and susceptible genes.
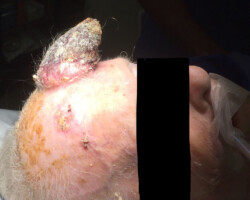
The staging of melanoma and risk of spread to other areas of the body is strongly correlated to the depth of invasion or thickness of the melanoma and presence of ulceration. This means that there is a defined risk of spread to the lymph nodes depending on the thickness of the melanoma. A melanoma up to 1 mm thick has a 5% risk, lesions 1 mm to 4 mm thick a 20% risk and lesions over 4 mm thick a 35% risk. Management guidelines include the ABCD criteria – Asymmetry, Border irregularity, Color variegation, Diameter increase.
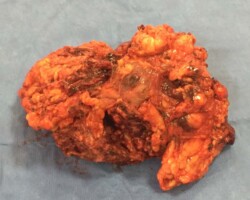
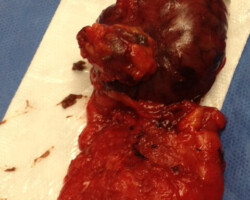
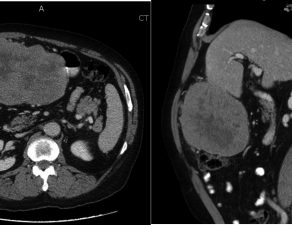
Patients should have an excisional biopsy performed by a dermatologist or surgeon followed by a careful pathology review. Proper excision and the need for sentinel lymph node biopsy are determined by depth and risk of spread. Other tests such as CT, PET, MRI and blood tests may be included.
We have the largest single practice performance of sentinel lymph node biopsies and dissections – over 2,000 in the past 14 years with advanced resections and reconstruction. Patients are presented at a multidisciplinary conferences weekly.